Reimbursement Support
Our living proof promise is to guide physicians and facilities through the reimbursement process, gain procedure access for patients who can benefit from the Intracept™ Procedure, and educate insurance companies along the way.
Reimbursement Support Center
Boston Scientific has a dedicated team of professionals to assist in the prior authorization of the Intracept™ Procedure. The prior authorization process involves obtaining advance notification from an insurance company that medical necessity and other coverage criteria have been met as set forth by the insurance company.
The Boston Scientific team works alongside the patient and physician throughout the prior authorization process in an attempt to obtain approval for the Intracept Procedure.
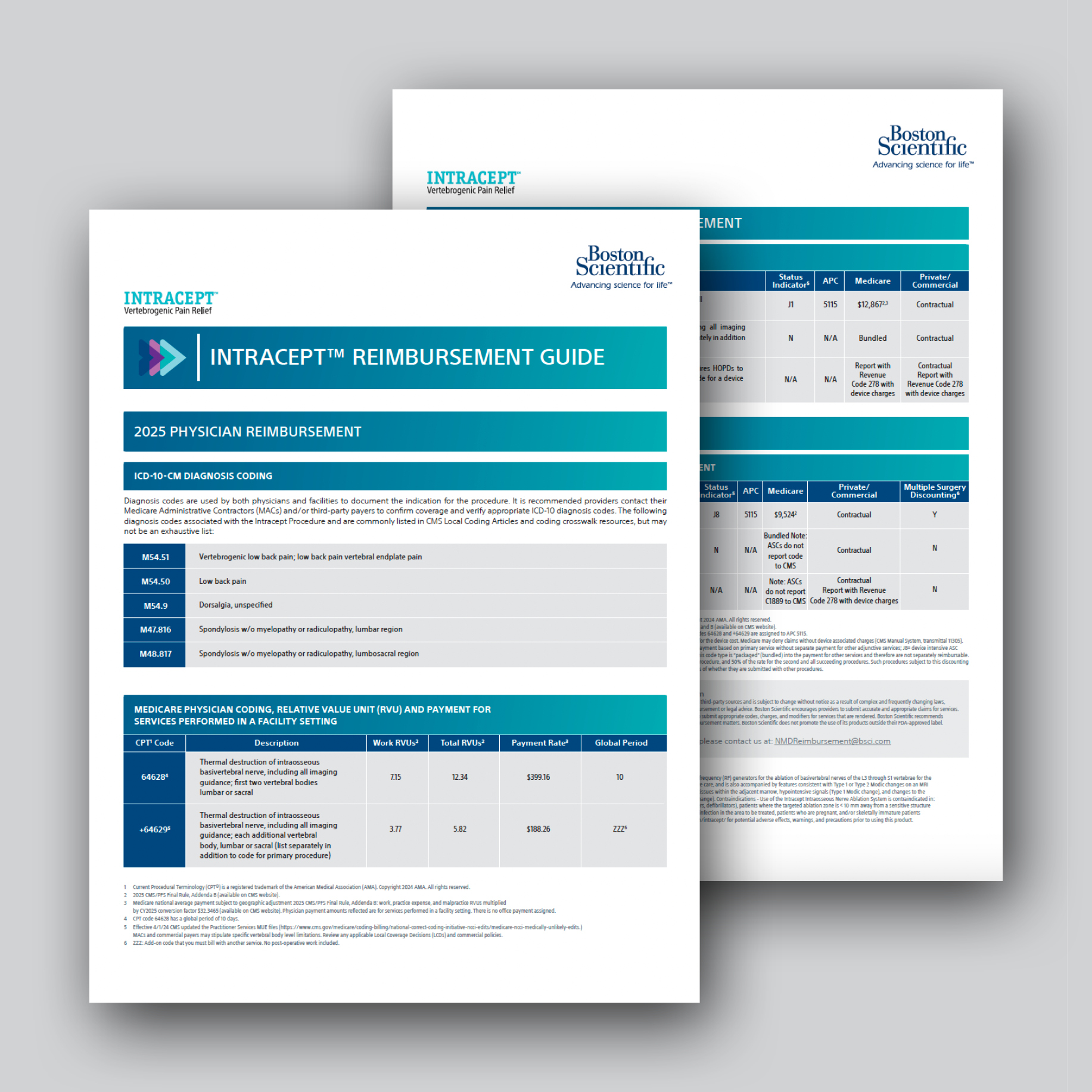
The Intracept™ Procedure is an outpatient procedure that is typically performed in either a hospital outpatient department (HOPD) or an ambulatory surgery center (ASC). As of January 1, 2022, two Category I Current Procedural Terminology (CPT) codes, 64628 and 64629, are in effect for the Intracept Procedure. Reimbursement by a payer will depend upon the contract with the facility.
Reimbursement Documents and Forms
2025 Reimbursement Guide for Physicians and Facilities
The Intracept™ Procedure is supported with Level l clinical evidence, has 510(k) Clearance, and is commercially available in the United States. For more information on the reimbursement support, please contact Boston Scientific reimbursement team at NMDReimbursement@bsci.com.
Boston Scientific is pleased to provide general information on coding, coverage and payment. This information is not intended to be legal or financial advice. Nothing stated above should be construed as a guarantee by Boston Scientific of coverage or payment for Intracept™ Procedures. Nothing should be viewed as an instruction to use a particular code or influence levels of payment. Providers are responsible for exercising their independent clinical judgment and reporting the codes that accurately reflect the patient’s condition and the services rendered and submit bills consistent with the patient’s insurer’s requirements. Reimbursement changes annually. This information is accurate as of January 1, 2025. Providers are advised to consult with the applicable payer or the specialty society or legal counsel for any coding, payment or billing related issues.

