Welcome to Living Proof
The Intracept™ Procedure is supported by strong scientific evidence, including two Level I randomized clinical trials. But the true proof is the living it has restored. You’ll find both kinds of proof here.
Looking for Proof?
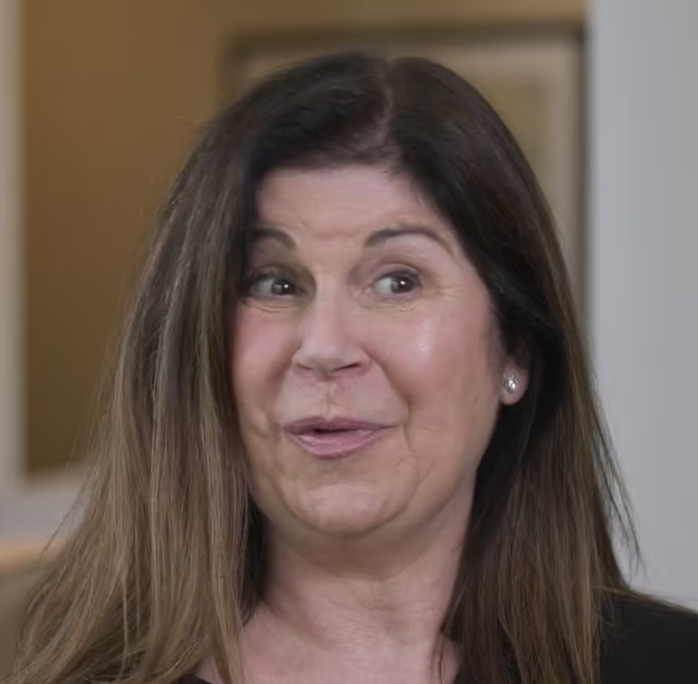
Hear from the Ones Living It.
Real Intracept Procedure patients tell their stories of lasting relief from vertebrogenic pain.
What Physicians Are Saying About Intracept
The Data Is Living Proof, Too
The Intracept™ Procedure is supported by unparalleled clinical evidence.
- Four clinical studies that include two Level I randomized controlled trials.
- Study results published in 10 peer-reviewed articles across 7 peer-reviewed journals, with additional systematic reviews and society guidelines on BVN ablation.
Proven Results
- Long-term improvements in pain and function, sustained more than 5 years1
- Sustained decrease in patients using opioids and injections long-term1
- Nearly 80% of patients indicated they would have the procedure again for the same condition1
- Less than 0.2% rate of serious device or procedure-related complications reported.2

Functional improvement.
Statistically sustained improvements in Oswestry Disability Index (ODI – a measure of function) shown 5 years post-procedure.1
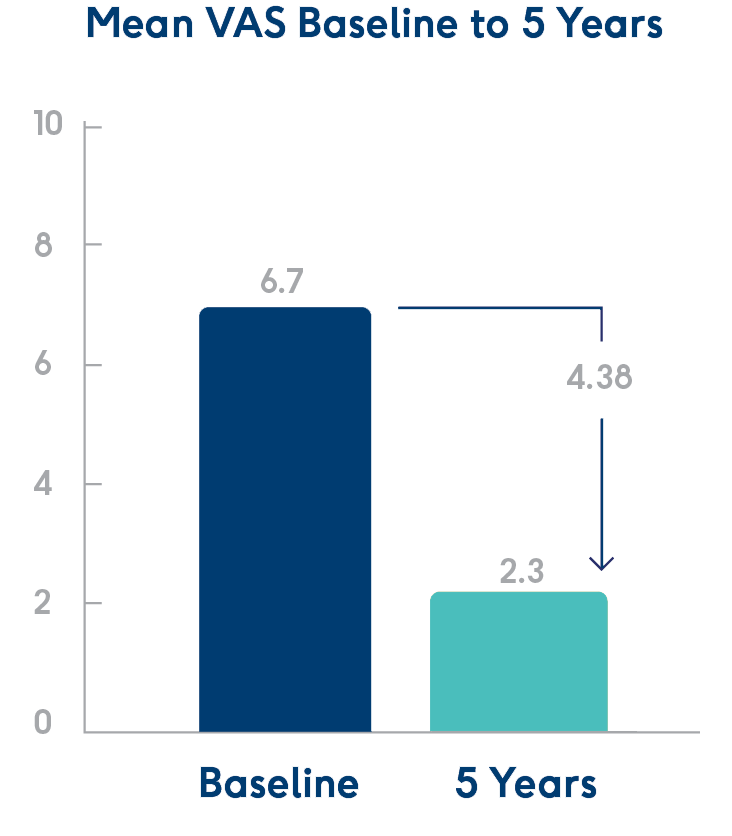
Pain reduction.
Statistically significant reductions in Visual Analog Scale (VAS – a measure of pain) shown 5 years post-procedure.1
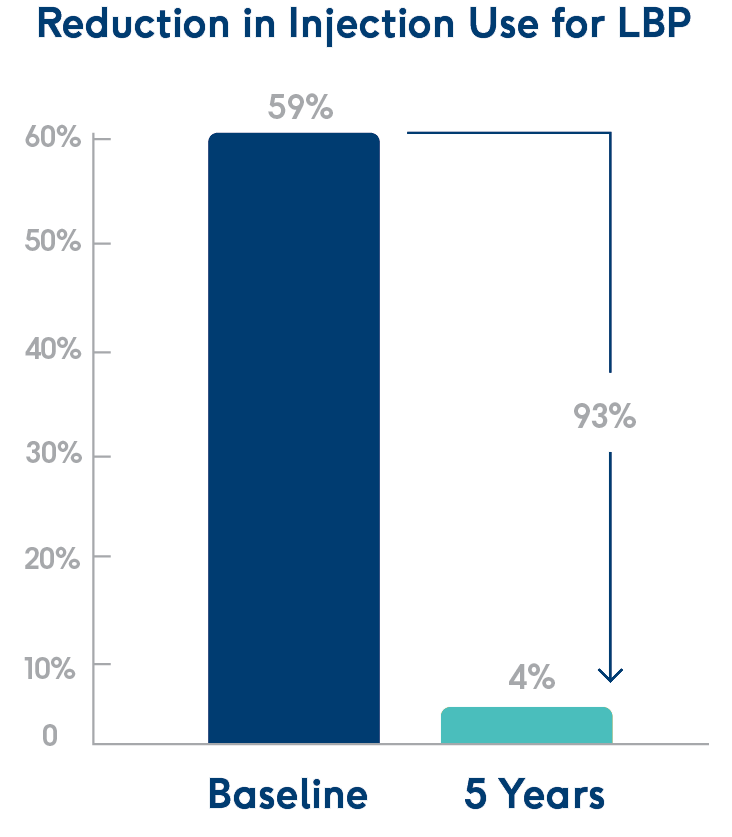
Fewer injections.
At 5 years post-procedure, 93% fewer patients had received injections.1
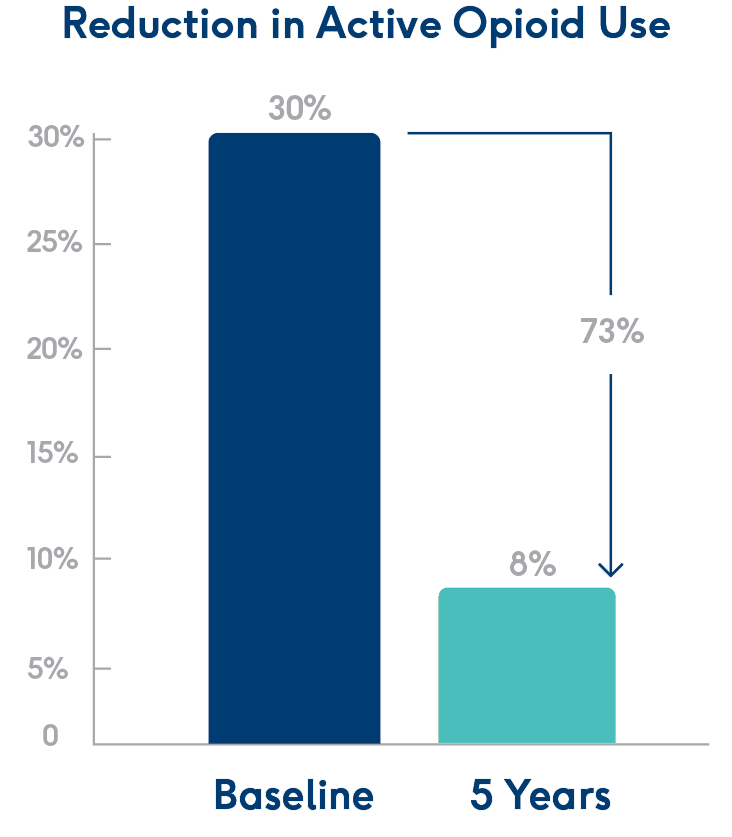
Fewer opioids.
At 5 years post-procedure, 73% fewer patients were actively using opioids.1
As with any surgical procedure, there are risks and considerations associated with the Intracept Procedure. See important safety information below.
Physicians: See Indications, Contraindications, and Risks
Indications for Use: The Intracept™ Intraosseous Nerve Ablation System is intended to be used in conjunction with radiofrequency (RF) generators for the ablation of basivertebral nerves of the L3 through S1 vertebrae for the relief of chronic low back pain of at least six months duration that has not responded to at least six months of conservative care, and is also accompanied by features consistent with Type 1 or Type 2 Modic changes on an MRI such as inflammation, edema, vertebral endplate changes, disruption and fissuring of the endplate, vascularized fibrous tissues within the adjacent marrow, hypointensive signals (Type 1 Modic change), and changes to the vertebral body marrow including replacement of normal bone marrow by fat, and hyperintensive signals (Type 2 Modic change). Contraindications - Use of the Intracept Intraosseous Nerve Ablation System is contraindicated in: Patients with severe cardiac or pulmonary compromise, patients with active implantable pulse generators (e.g. pacemakers, defibrillators), patients where the targeted ablation zone is < 10 mm away from a sensitive structure not intended to be ablated, including the vertebral foramen (spinal canal), patients with active systemic infection or local infection in the area to be treated, patients who are pregnant, and/or skeletally immature patients (generally ≤ 18 years of age). Refer to the Instructions for Use provided with the Intracept Procedure or www.relievant.com/intracept/ for potential adverse effects, warnings, and precautions prior to using this product.
Caution: U.S. Federal law restricts this device to sale by or on the order of a physician.
Copyright © 2025 by Boston Scientific Corporation or its affiliates. All rights reserved.
Patients: See the Indications & Risks Involved
Contraindications include being pregnant, having weakened cardiac or pulmonary function, having an active implanted electronic medical device in the body (such as a pacemaker or defibrillator), being diagnosed with a systemic or local infection, or having an anatomy that could be damaged unintentionally while ablating the basivertebral nerve (based on your physicians’ clinical review). The Intracept Procedure is also contraindicated in patients who are skeletally immature – which generally means individuals under the age of 18 are not candidates. There are also certain risks and precautions regarding the procedure which you should be aware of before proceeding. Talk with your doctor about what indicates, and contraindicates, certain patients for the Intracept Procedure – as well as the risks and precautions for the procedure. For complete indications for use, contraindications, warnings, precautions, and side effects visit www.relievant.com/intracept/.
Caution: U.S. Federal law restricts this device to sale by or on the order of a physician.
Copyright © 2025 by Boston Scientific Corporation or its affiliates. All rights reserved.
- Fischgrund J, Rhyne A, Macadaeg K, et al. Long-term outcomes following intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 5-year treatment arm results from a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2020;29(8):1925-34. doi.org/10.1007/s00586-020-06448-x
- Data on file.
NM-2011812-AA