Saying Yes to Life and to Lasting Pain Relief
That’s the living proof of the Intracept™ Procedure: The only targeted way to relieve vertebrogenic chronic low back pain (CLBP). Here’s the basics:
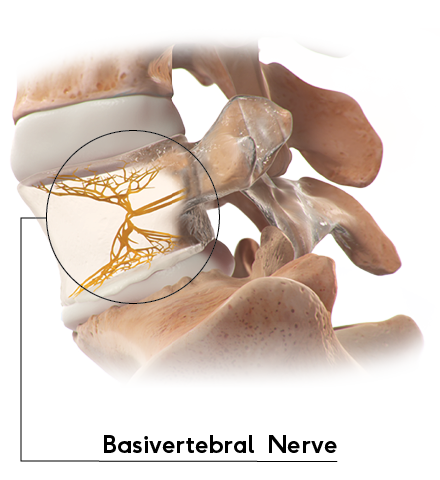
A Certain Nerve Is the Key
Vertebral endplates – found on either side of the disc – can become damaged over time, causing inflammation and back pain. The basivertebral nerve (BVN), found within the vertebrae, carries these back pain signals from the inflamed endplates to the brain.
The Intracept™ Procedure Can Relieve the Pain
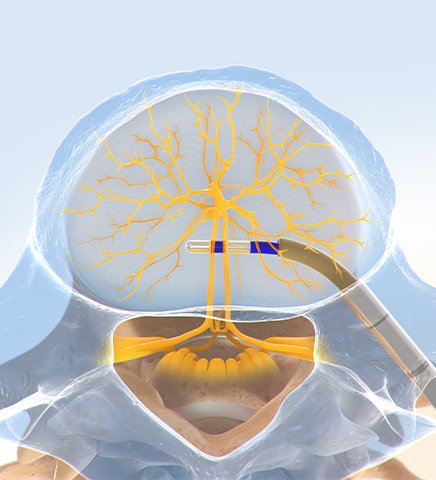
The Intracept Procedure is a same-day procedure performed in an outpatient surgery center. Unlike some major surgeries, the Intracept Procedure is implant-free and preserves the overall structure of the spine.
The Intracept Procedure involves heating the basivertebral nerve with a radiofrequency probe to stop it from sending pain signals to the brain. Patients are under anesthesia, and the procedure generally lasts an hour.
Different from other nerves in the body that regenerate, the BVN has not shown an ability to grow back as a pain-transmitting nerve following the Intracept Procedure.
What to Expect After the Procedure
Lasting Pain Relief
Patients in a recent study reported their improvements in function and pain relief lasted more than 5 years following the procedure – with over a third of these patients indicating they were totally pain-free.1
As with any surgical procedure, there are risks and considerations associated with the Intracept Procedure. See important safety information below.
Physicians: See Indications, Contraindications, and Risks
Indications for Use: The Intracept™ Intraosseous Nerve Ablation System is intended to be used in conjunction with radiofrequency (RF) generators for the ablation of basivertebral nerves of the L3 through S1 vertebrae for the relief of chronic low back pain of at least six months duration that has not responded to at least six months of conservative care, and is also accompanied by features consistent with Type 1 or Type 2 Modic changes on an MRI such as inflammation, edema, vertebral endplate changes, disruption and fissuring of the endplate, vascularized fibrous tissues within the adjacent marrow, hypointensive signals (Type 1 Modic change), and changes to the vertebral body marrow including replacement of normal bone marrow by fat, and hyperintensive signals (Type 2 Modic change). Contraindications - Use of the Intracept Intraosseous Nerve Ablation System is contraindicated in: Patients with severe cardiac or pulmonary compromise, patients with active implantable pulse generators (e.g. pacemakers, defibrillators), patients where the targeted ablation zone is < 10 mm away from a sensitive structure not intended to be ablated, including the vertebral foramen (spinal canal), patients with active systemic infection or local infection in the area to be treated, patients who are pregnant, and/or skeletally immature patients (generally ≤ 18 years of age). Refer to the Instructions for Use provided with the Intracept Procedure or www.relievant.com/intracept/ for potential adverse effects, warnings, and precautions prior to using this product.
Caution: U.S. Federal law restricts this device to sale by or on the order of a physician.
Copyright © 2025 by Boston Scientific Corporation or its affiliates. All rights reserved.
Patients: See the Indications & Risks Involved
Contraindications include being pregnant, having weakened cardiac or pulmonary function, having an active implanted electronic medical device in the body (such as a pacemaker or defibrillator), being diagnosed with a systemic or local infection, or having an anatomy that could be damaged unintentionally while ablating the basivertebral nerve (based on your physicians’ clinical review). The Intracept Procedure is also contraindicated in patients who are skeletally immature – which generally means individuals under the age of 18 are not candidates. There are also certain risks and precautions regarding the procedure which you should be aware of before proceeding. Talk with your doctor about what indicates, and contraindicates, certain patients for the Intracept Procedure – as well as the risks and precautions for the procedure. For complete indications for use, contraindications, warnings, precautions, and side effects visit www.relievant.com/intracept/.
Caution: U.S. Federal law restricts this device to sale by or on the order of a physician.
Copyright © 2025 by Boston Scientific Corporation or its affiliates. All rights reserved.
- Fischgrund J, Rhyne A, Macadaeg K, et al. Long-term outcomes following intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 5-year treatment arm results from a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2020;29(8):1925-34. http://doi.org/10.1007/s00586-020-06448-x

