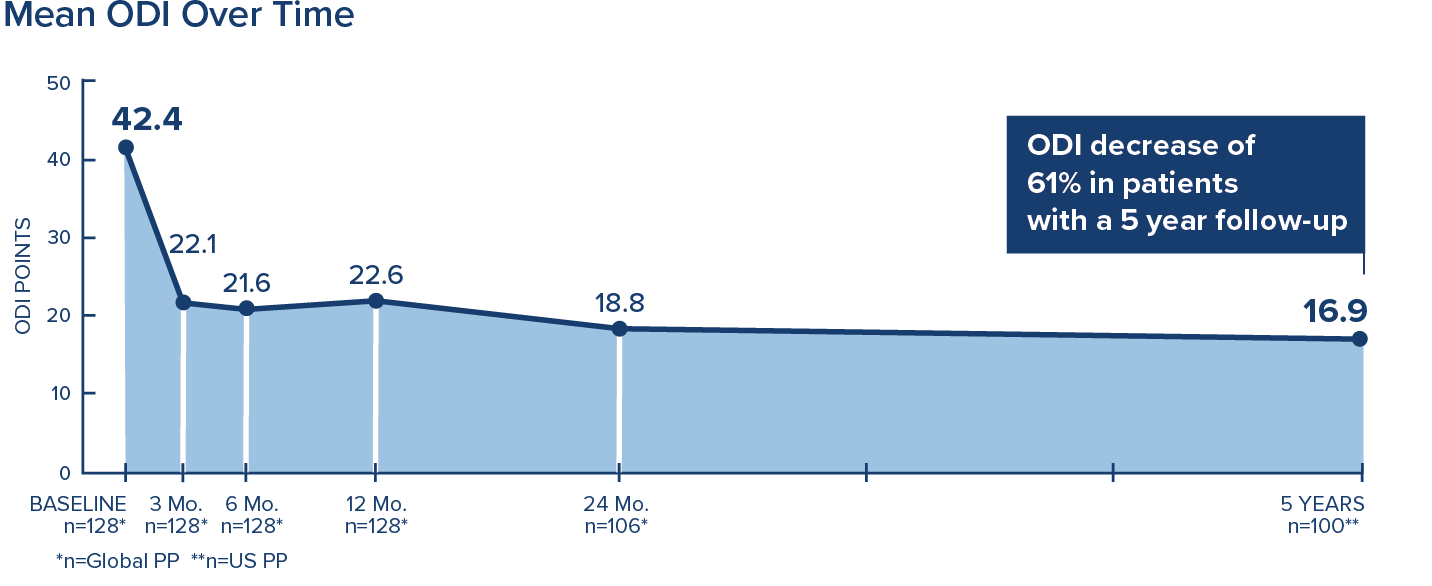
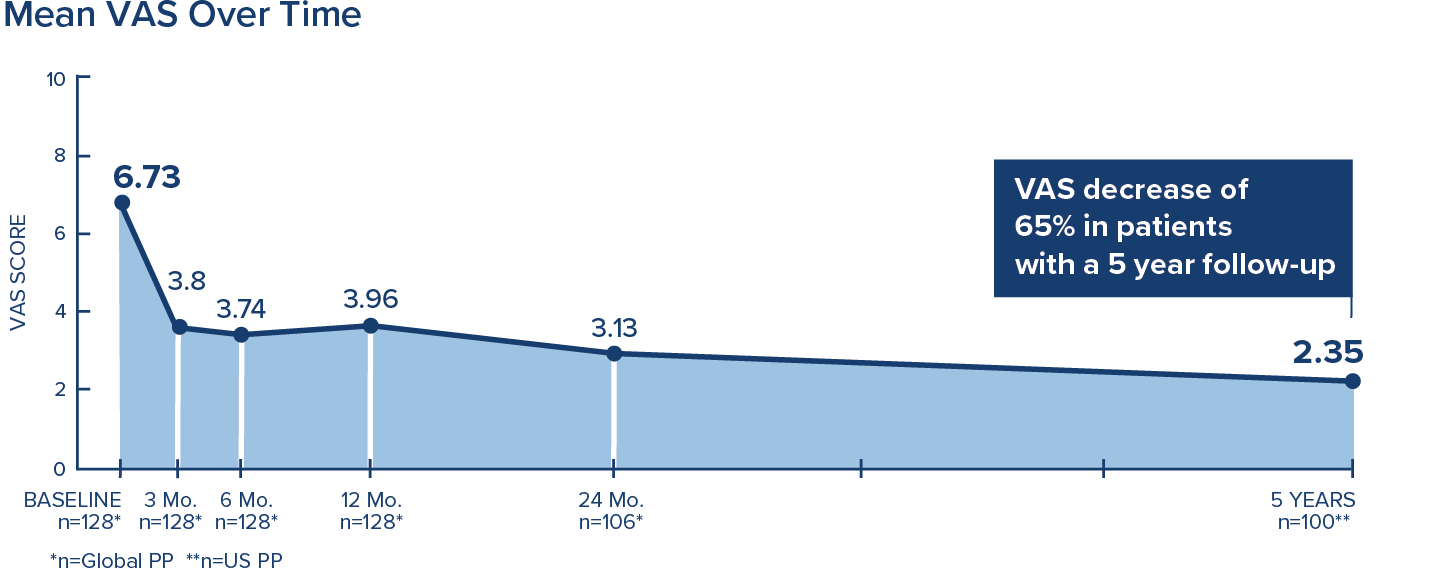
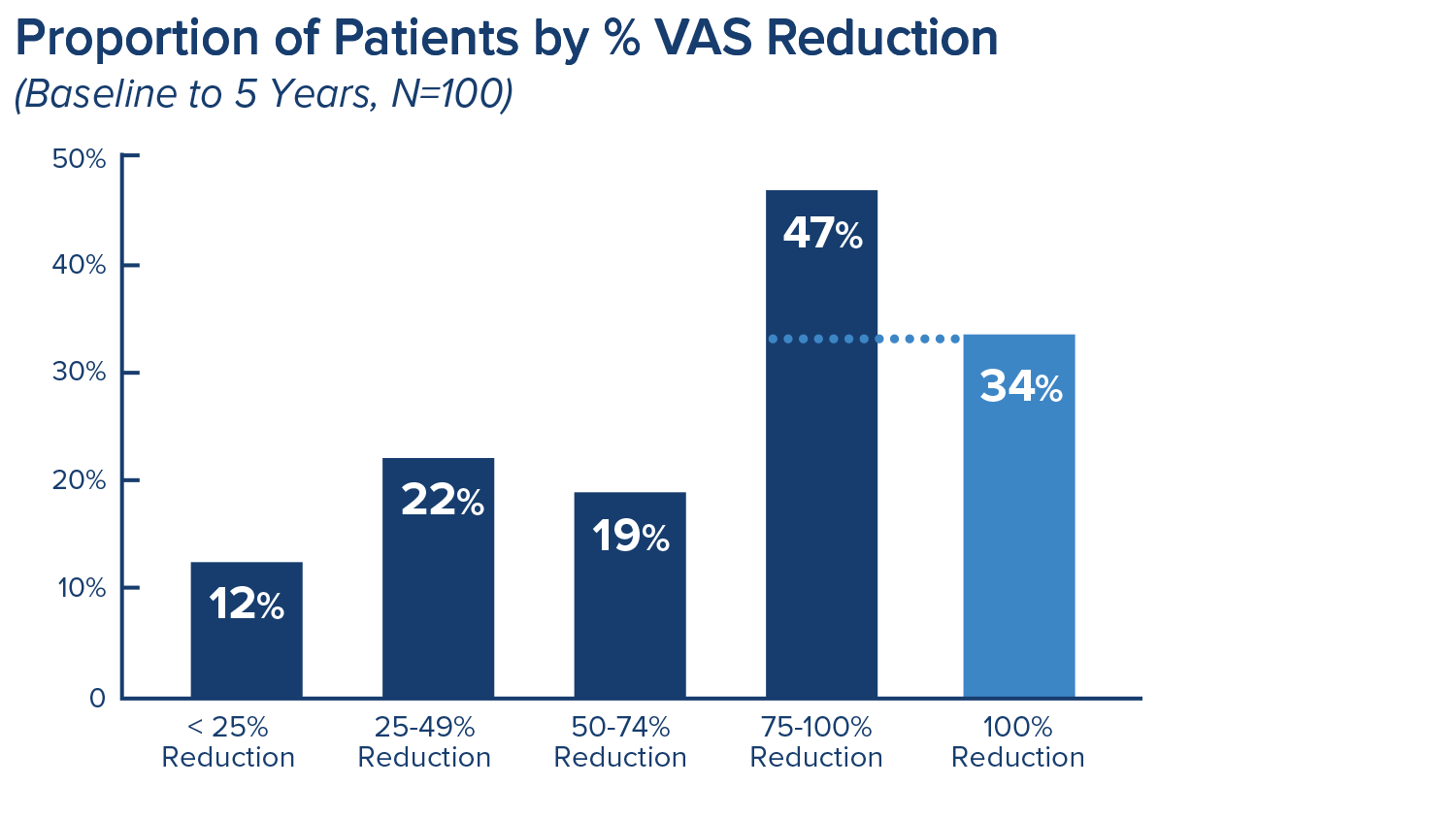
Long-Term Relief
5-Year Durability3
Purpose
Study Design
- Prospective five year follow-up of the SMART US treatment arm patients 1, 2, 3
- All 13 US treating sites participated
- Retention rate of 85% per protocol treatment arm population (n=100) (PP = Per Protocol)
- Mean follow-up of 6.4 years (range 5.4 to 7.8 years posttreatment)
Key Findings
Conclusion
1. Fischgrund JS, Rhyne A, Franke J, Sasso R, Kitchel S, Bae H, et al. Intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2018;27(5):1146-56.
2. Fischgrund JS, Rhyne A, Franke J, et al. Intraosseous Basivertebral Nerve Ablation for the Treatment of Chronic Low Back Pain: 2-Year Results from a Prospective Randomized Double-Blind Sham-Controlled Multicenter Study. International Journal of Spine Surgery, Vol. 13, No. 2, 2019, pp. 1–10.
3. Fischgrund JS, Rhyne A, Macadaeg K, Moore G, Kamrava E, Yeung C, et al. Long-term outcomes following intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 5 year treatment arm results from a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. epub May 25, 2020.
*The intent-to-treat (ITT) population consisted of the patients as randomized and the per-protocol (PP) population excluded any patients in which the procedure could not be carried out, RF generated lesion did not colocate with BVN terminus or who were not compliant with the post-operative protocol.

